Blog
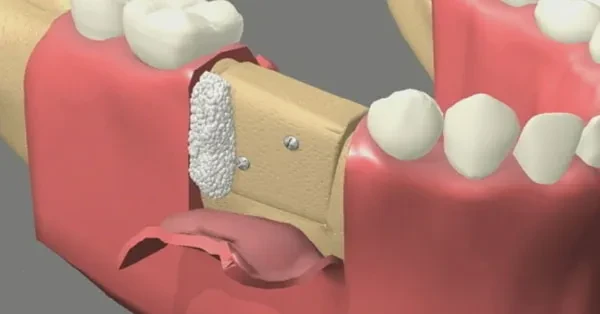
Overview of Risks and Benefits of Bone Grafting in Washington
July 17, 2025Bone grafting might sound like something from a medical drama, but for many patients in Washington, it’s the essential first step toward restoring a full, healthy...
Overview of Risks and Benefits of Bone Grafting in Washington Read more
Top Questions to Ask About Sedation Dentistry in Washington
July 17, 2025Feeling anxious about an upcoming dental procedure? You’re not alone. Sedation dentistry has become an increasingly popular solution for patients who want a ...
Top Questions to Ask About Sedation Dentistry in Washington Read more
Healing Timeline for Dental Implants in Washington
June 21, 2025Dental implants represent an extended investment in your smile and dental well-being. If you're planning to undergo the procedure, one of the most common questions...
Healing Timeline for Dental Implants in Washington Read more
Recovery Tips After Sedation Dentistry in Washington
June 21, 2025Undergoing a dental procedure involving sedation can be a significant step toward restoring your oral health, whether you're getting a simple extraction, dental implants,...
Recovery Tips After Sedation Dentistry in Washington Read more
Debunking the Top Myths About Sedation Dentistry in Washington
May 14, 2025For many people, visiting the dentist can feel like a nerve-wracking experience. Whether it's due to fear of pain, prior trauma, or general anxiety...
Debunking the Top Myths About Sedation Dentistry in Washington Read more
Choosing the Right Surgeon for Dental Implants in Washington
May 14, 2025When considering tooth replacement options, dental implants are one of the most effective, long-lasting solutions available. However, the outcome of your...
Choosing the Right Surgeon for Dental Implants in WashingtonRead more
Wisdom Teeth Removal with Sedation Dentistry in Washington
April 14, 2025Wisdom teeth removal can be a daunting experience, especially for patients who experience dental anxiety or anticipate pain during oral surgery. Fortunately...
Read more
5 Common Myths About Dental Implants in Washington
April 14, 2025When restoring a confident smile, dental implants are one of the most popular and reliable solutions available today. Yet, despite their increasing popularity...
Read more
Top 6 Recovery Tips for Dental Implants in Washington
March 18, 2025Getting dental implants is a great way to restore your smile and improve your oral health. However, the recovery process plays a crucial role in ensuring successful...
Read more
5 Common Concerns About Sedation Dentistry in Washington
March 18, 2025Sedation dentistry is a game-changer for patients who experience anxiety when visiting the dentist. Whether you need a routine cleaning or a complex procedure...
Read more
5 Nutrition Tips Post-Dental Implants in Washington
February 19, 2025Getting dental implants is a transformative step toward restoring your smile and confidence. While the procedure itself is highly advanced, your post-surgery care plays a crucial role...
Read more
5 Key Signs You Need Dental Implants in Washington
February 03, 2025When it comes to restoring your smile and improving your quality of life, dental implants are are one of the most effective and long-lasting solutions. If you...
Read more
Discover 4 Different Types of Dental Implants in Washington
December 26, 2024Dental implants are transforming smiles and redefining confidence, providing patients with a dependable and visually appealing solution...
Read more
Wisdom Teeth Removal in Washington: Recovery Timeline
October 1, 2024Wisdom teeth removal is a common dental procedure that many individuals in Washington undergo to prevent future complications like.......
Read more
Overcoming Dental Anxiety with Sedation Dentistry in Washington
October 1, 2024Dental anxiety is a common issue that affects many individuals, making routine visits to the dentist a daunting experience. However, sedation dentistry.......
Read more
5 Key Benefits of Choosing Dental Implants in Washington
October 1, 2024When it comes to replacing missing teeth, dental implants are an increasingly popular choice for individuals in Washington. Not only do they offer a long-lasting and natural.......
Read more
Sedation Dentistry: Types, Procedure, and What to Expect
October 26, 2023Wisdom teeth, scientifically known as third molars, have intrigued and sometimes inconvenienced people worldwide. These late-blooming teeth often.......
Read more
Why Do We Have Wisdom Teeth? Exploring Their Evolution and Removal!
October 18, 2023Wisdom teeth, scientifically known as third molars, have intrigued and sometimes inconvenienced people worldwide. These late-blooming teeth often.......
Read more
What Drug is Used for IV Sedation in Dentistry?
October 17, 2023When it comes to dental procedures, sedation dentistry, anxiety, and fear are common sentiments among patients. These emotions often deter individuals.......
Read more
What to Eat After Wisdom Teeth Removal?
October 16, 2023Wisdom teeth removal in Washington is a common dental procedure that many patients in Washington undergo at some point in their lives. This surgical process involves the.......
Read more
The Dangers of Ignoring Impacted Wisdom Teeth in Washington
October 13, 2023Wisdom teeth, often called third molars, are notorious for causing discomfort and dental problems. When it's time to address these issues.......
Read more
The Dangers of Ignoring Impacted Wisdom Teeth in Washington
October 11, 2023It's all too easy to overlook the silent threat of impacted wisdom teeth when surrounded by the beauty of nature.......
Read more
What to Eat and Drink Before and After Sedation Dentistry in Washington?
October 11, 2023For people who are anxious about going to the dentist or who avoid doing so, sedation dentistry in Washington has completely changed the dental experience......
Read more
Tips for Managing Wisdom Teeth Removal Anxiety in Washington
October 11, 2023The third molars, commonly referred to as wisdom teeth, are the ones that arrive later in life and typically erupt in the late teens or early twenties.....
Read more
What to Expect Before, During, and After a Bone Grafting Surgery in Washington
September 30, 2023Is bone grafting in Washington anything you're thinking about? Understanding the process is essential for a successful outcome ....
Read more
Bone Grafting vs. Sinus Lift: Which Procedure is Right for You in Washington?
September 30, 2023Bone grafting in Washington and sinus lifts are two treatments that are frequently used to treat jaw bone loss. Which of these operations is best for you....
Read more
Choosing the Right Dental Surgeon for Bone Grafting in Washington
September 30, 2023A confident smile is a treasure, and choosing the best dental surgeon is crucial when it comes to repairing bone grafting in Washington....
Read more
Comprehensive Oral Surgery Services in Washington: Everything You Need to Know
September 04, 2023Sedation dentistry in Washington provides a wide range of therapies for maintaining oral health, including wisdom teeth removal and dental implants...
Read more
Can General Dentists Perform Oral Surgery Procedures?
September 04, 2023There's a common misconception that general dentists lack the training to perform complex oral surgical procedures such as dental implants, wisdom teeth removal,..
Read more
The Benefits of Sedation Dentistry for a Smooth Wisdom Teeth Removal
September 04, 2023"Third Molars," commonly referred to as Wisdom Teeth, represent the final set of teeth that develop in adults....
Read more
The Science Behind Sedation: How Your Body Responds to Dental Anxiety
August 24, 2023Are you thinking about getting dental implants to bring back your smile and boost your confidence? The field of dentistry has undergone..
Read more
The Role of Bone Grafting for Dental Implants in Washington
August 18, 2023Are you thinking about getting dental implants to bring back your smile and boost your confidence? The field of dentistry has undergone..
Read more
Wisdom Teeth Removal Recovery: Key Steps and Considerations
August 11, 2023Wisdom teeth removal is a common dental procedure, often necessary to prevent complications and maintain oral health...
Read more
A Patient’s Guide to the Cost of Dental Implant Surgery
May 27, 2022Whether you’ve been missing a few teeth for a while or you have to get an infected tooth removed soon, you might be interested in some ways to restore your smile...
Read more
Explaining Each Part of Your Wisdom Tooth Surgery Bill
May 12, 2022The cost of wisdom teeth removal can vary depending on a number of factors, including the type of extraction and the credentials of your provider...
Read more
Worth the Cost: How Oral Surgery Helps Avoid Emergencies in the Long Run
April 28, 2022Oral surgery is essential for many dental concerns, and delaying these procedures doesn’t just mean the problem will continue...
Read more
Oral Surgery for Gum Disease: A Patient’s Guide
April 14, 2022Gum disease can eventually eat away at the teeth and jawbone, so in instances like these, an oral surgeon may need to perform one or more procedures...
Read more
Top 5 Tips for Recovering from Oral Surgery
April 01, 2022In order to have a speedy oral surgery recovery with less chance of complications, you should follow your oral surgeon’s instructions, eat properly...
Read more
The Five Most Important Tools to Have in Your Medicine Cabinet to Ensure a Healthy Smile
March 14, 2022The top five most important tools to have in your medicine cabinet to safeguard your smile’s health...
Read more
Understanding the Causes and Risks of Gum Disease
March 01, 2022Periodontitis can lead to the destruction of soft tissue and bones that support the teeth, causing loose teeth and tooth loss. Tooth loss is irreversible...
Read more
Want a Bright and Healthy Smile? Follow These Top Tips
February 10, 2022A bright and healthy smile starts at home. Seeing your dentist every six months for a routine cleaning and checkup is a big step in the right direction...
Read more
Six Questions to Ask Your Oral Surgeon Before a Procedure
January 27, 2022Whether you were referred to Oral Surgery DC by your regular dentist or you are interested in an elective treatment, knowing what to expect...
Read more
A Patient’s Guide to Preventing Tooth Loss
January 13, 2022If you want to ensure tooth loss prevention, even as you age, learn the basics of dental care, what tooth loss treatment looks like...
Read more
How To Tell If You Need an Oral Surgeon Or a Dentist
December 30, 2021Oral surgeons can assist in providing treatment for many dental procedures that cannot be performed by regular dentists...
Read more
A Patient’s Guide to Choosing an Oral Surgeon
December 16, 2021Before choosing an oral surgeon to perform your oral surgery, you should consider several factors. Doing so ensures you...
Read more
The Why’s and How’s of Adult Wisdom Tooth Extraction
December 01, 2021Adult wisdom tooth extraction is often more complex than removing wisdom teeth at a younger age and requires the expertise of an oral surgeon...
Read more
Understanding Tooth Loss and Your Oral Surgery Treatment Options
October 13, 2021According to the American College of Prosthodontists, approximately 178 million Americans have lost at least one...
Read more
Cosmetic and Reconstructive Surgery: What Can An Oral Surgeon Do to Help?
October 06, 2021Whether an injury or medical condition has harmed the structures of your face and jaw and reduced their functionality...
Read more
A Guide to Caring for Your Dental Implants
September 29, 2021Dental implants work and feel just like your own teeth, but these marvels of oral surgery require the same hygiene and maintenance as your natural teeth. Take heed of these useful dental implant care tips...
Read more
Dental Implants: A Great Alternative to Dentures and Bridges
September 22, 2021Dental implants are many patients’ best option for tooth replacement. Dentures and other replacement solutions are often uncomfortable...
Read more
All You Need to Know About Sedation Dentistry
September 14, 2021If you always had trouble remaining calm for dental appointments, or if you grow anxious at the prospect of major procedures such as dental implants, sedation dentistry can help you feel at ease...
Read more
Five Steps You Can Take to Prepare Successfully for Your Oral Surgery Procedure
August 25, 2021If you require oral surgery, it is important to take proactive action. Surgery preparation will reduce your risk of complications while increasing the rate of recovery...
Read more
When and Why Your Dentist Will Refer You to an Oral Surgeon
May 14, 2021When it comes to the health of your mouth, it’s important to know which type of professional is best suited to handle the particular issues you are facing. Dentists focus on preventative care...
Read more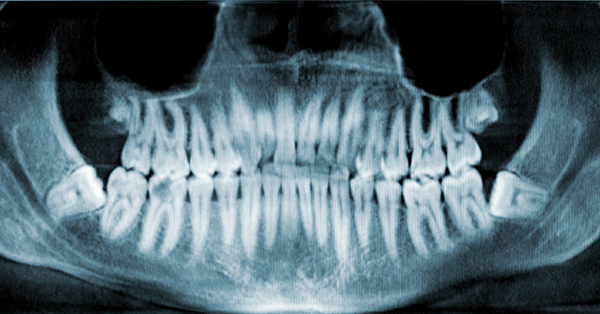
Impacted Teeth: What You Need to Know for Successful Removal and Recovery
April 21, 2021Impacted teeth are pretty common, and happen with a tooth that doesn’t grow out, or erupt, naturally continues growing under the gum instead...
Read more
Top 5 Tips for Recovering from Oral Surgery
April 21, 2021In order to have a speedy oral surgery recovery with less chance of complications, you should follow your oral surgeon’s...
Read more
Making the Most of Your Smile: Healthy Habits that Protect Your Teeth
March 11, 2021Practicing basic dental hygiene can increase your overall wellbeing...
Read more
Oral Surgery for Gum Disease: A Patient’s Guide
March 10, 2021Gum disease can eventually eat away at the teeth and jawbone, so in instances like these, an oral surgeon may need to perform...
Read more
Understanding the Causes and Risks of Gum Disease
February 24, 2021Periodontitis can lead to the destruction of soft tissue and bones that support the teeth, causing loose teeth and tooth loss...
Read more
6 Ways Oral Surgeons Can Help Improve Your Quality of Life
February 22, 2021Oral surgeons can help you improve your quality of life in a wide variety of situations, including dental implants...
Read more
What is Diastema?
March 29, 2020By: Jayne Leonard, Medical News Today A diastema is a gap between the teeth. It is not harmful, and it appears in children and adults. In children, the gap typically closes when their permanent teeth come through...
Read more
Vaping changes oral microbiome and raises infection risk
March 23, 2020By: Eleanor Bird, M.S., Medical News Today Researchers from New York University (NYU) College of Dentistry are the first to show that the use of e-cigarettes...
Read more
Notice: Rescheduling Elective Dental Procedures
March 17, 2020The Maryland State Dental Association and the American Dental Association issued guidelines that elective dental procedures should be put off until at least April 1st...
Read more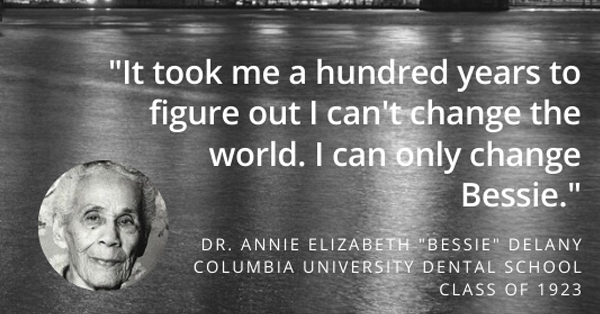
Black History Month Spotlight: Dr. Annie Elizabeth “Bessie” Delany
February 20, 2020For Black History Month, we’d like to pay tribute to trailblazers and honor lesser-known people of color in the dental and oral surgery fields...
Read more
Can Wisdom Teeth Cause Headache Pain?
February 05, 2020Article written by: Healthline Headaches can be traced to a variety of causes, including wisdom teeth that are emerging...
Read more
4 Home Remedies For Abscessed Teeth
January 28, 2020Article Written By: Amy Freeman, Colgate You’re experiencing some serious pain in your mouth, and you think a dental abscess...
Read more
How Oral Health And Heart Disease Are Connected
January 22, 2020Article written by: Tracey Sandilands | Colgate It’s increasingly common to hear that oral health is vital for overall health...
Read more
What to Eat After Wisdom Teeth Removal
January 01, 2020By: Ana Gotter, Healthline Most people heal quickly from wisdom teeth removal, as long as they follow the doctor’s instructions during recovery...
Read more
TMJ and Jaw Pain – Why Does My Jaw Hurt?
December 28, 2019By: 123 Dentist Trauma, dental problems, and other health conditions can cause jaw pain. Pain in the jaw can range from uncomfortable to extreme...
Read more
Dentist or Detective? Major Health Clues Your Mouth Provides
November 02, 2019Chew on this for a minute: just by glancing inside your mouth, your dentist can tell you a number of things...
Read more
The Story on Soda: Your Soft Drink Questions Answered
October 30, 2019Sorry to burst your bubble, but the reality is that no matter how refreshing that sweet, fizzy soda (or “pop”) tastes, there’s a chance it could be doing some damage...
Read more
Sealants: Stop Cavities Before They Begin
October 26, 2019Aside from proper brushing and flossing to remove food particles and plaque from smooth surfaces of teeth, do you know that there are other effective ways...
Read more
How to Get Whiter Teeth: Four Top Tips to Help Achieve a Brighter Smile
October 23, 2019By: Matty Edwards, Independent ? What does good oral hygiene mean for you? Aside from brushing, keeping our teeth...
Read more
Drinking Red Wine Can Improve Oral Hygiene, Study Claims
October 19, 2019By: Olivia Petter, Independent DYK? Drinking red wine can improve your oral health!? So, how about wine-flavored toothpaste?...
Read more
More than a smile: Importance of your kid’s long-term oral health
October 16, 2019By: CNN Philippines ? Busy days at work and school can hamper our oral care routine. Children, in particular...
Read more
Dentist or Detective? Major Health Clues Your Mouth Provides
October 07, 2019Chew on this for a minute: just by glancing inside your mouth, your dentist can tell you a number of things that may be news...
Read more
The Story on Soda: Your Soft Drink Questions Answered
September 30, 2019Sorry to burst your bubble, but the reality is that no matter how refreshing that sweet, fizzy soda (or “pop”) tastes...
Read more
Sealants: Stop Cavities Before They Begin
September 24, 2019Aside from proper brushing and flossing to remove food particles and plaque from smooth surfaces of teeth...
Read more
In Defense of Root Canals: The Unsung Hero of Dental Care
September 17, 2019Think you might need a root canal? It’s not the end of the world, nor is it as torturous as you might think!...
Read more
A Visibly Straighter Smile with Invisible Orthodontics
September 10, 2019Think you might need a root canal? It’s not the end of the world, nor is it as torturous as you might think!...
Read more
Smoking, Your Mouth, and Your Health
September 03, 2019There are no ifs, ands, or “butts” about it: smoking can be detrimental to oral health. Beyond the bad breath and yellow teeth...
Read more
A Child’s First Visit to the Dentist
September 03, 2019It can be shocking to many parents, if not perplexing: many dentists now recommend you schedule your child’s first visit...
Read more
‘Inadequate’ health response leaves 3.5bn with poor dental care
August 10, 2019By: Sarah Boseley, The Guardian ⚠️ Scientists are calling for radical reform of dental care, tighter regulation of the sugar industry...
Read more
How Did People Clean Their Teeth in the Olden Days?
August 03, 2019By: The Conversation, AP News, Snopes [FUN FACT] Dental hygiene has come a long way since the days of wine-soaked toothpicks...
Read more
Dental Hygiene for Infants to Preteens
July 27, 2019By: Bingham Healthcare, Post Register. Your child’s well-being is your biggest concern and their oral hygiene is an important part of their overall health...
Read more
10 common oral hygiene mistakes, according to dentists
July 20, 2019By: Wendy Rose Gould, NBC News ? According to the CDC, more than 80% of people develop at least one cavity by age 34...
Read more
What You Can Do About Bad Breath
July 13, 2019By: Peter Jaret, WebMD Don’t be afraid to get a little close this National Fresh Breath Day! Check out the 8 natural ways to freshen your breath?...
Read more
A Visibly Straighter Smile with Invisible Orthodontics
July 06, 2019The invisible orthodontics is one of the leading alternatives for both teenagers and adults. While the primary reason many choose this option is that they don’t like the appearance of metal braces...
Read more
In Defense of Root Canals: The Unsung Hero of Dental Care
June 29, 2019Think you might need a root canal? It’s not the end of the world, nor is it as torturous as you might think! Even though a root canal is usually the last resort for decayed teeth...
Read more
Thrush — the White Stuff Growing in Your Mouth (and How to Get Rid of it)
June 22, 2019By: Cleveland Clinic. What’s that white stuff on your tongue? And why does your mouth feel “funny” — maybe a little bit like sandpaper?...
Read more
Brushing and Flossing Could Reduce Your Risk of This Cancer
June 15, 2019By: Lara DeSanto, HealthCentral Do you know that improper dental care and hygiene can increase your risk of developing liver cancer?...
Read more
Oral Piercings: What You Should Know
June 08, 2019By: WebMD While piercing the tongue, lip or cheek may be attractive to some, there are a number of health-related risks associated with oral piercing...
Read more
Understanding Pediatric Fluoride Treatment
June 01, 2019It’s undeniable that fluoride has played a major role in the decline of dental cavities in the United States. However, what isn’t so clear to many parents...
Read more
Dental infections in kids tied to heart disease risk in adulthood
May 22, 2019Children who develop cavities and gum disease may be more likely to develop risk factors for heart attacks and strokes decades later than kids...
Read more
Dentists without drills: Minimally invasive dentistry is on the rise
May 15, 2019By: Katharine Gammon, USC News ? Are you afraid to go to the dentist or do you have phobia on dental drills? Well, not anymore!...
Read more
Genetic make-up has little impact on dental health, a new study finds
May 09, 2019By: University of Melbourne, Medical Xpress ? A new study has found genetic makeup does not predispose people to tooth...
Read more
Charcoal Kinds of Toothpaste ‘Don’t Whiten Teeth’
May 02, 2019By: BBC News ⚠️ Charcoal-based toothpaste, which claims to whiten teeth, is a “marketing gimmick” which could increase the risk of tooth decay...
Read more
Oral cancer: What you can do to help end this disease
April 27, 2019By: American Dental Association, ASDA ? The American Cancer Society estimates there will be 53,000 new cases of oral and oropharyngeal cancer in 2019...
Read more
Do You Know The Importance Of Family Dental Care?
April 20, 2019By: Longevity Most of us are well-versed with the fact that dental care is important. But why exactly it is so important, is something which a majority of us...
Read more
What Dental Issues Can Women Face during Pregnancy?
April 14, 2019By: Lucy Wyndham, Dental News ? Pregnancy brings about many changes in your body, but one which you may not necessarily...
Read more
What to know about gargling with salt water
April 06, 2019By: Jenna Fletcher, Medical News Today. Sore throats and mouth sores are common conditions that most people experience.? Do you know that saltwater gargles can be a cheap, safe...
Read more
Oral cancer: What you can do to help end this disease
March 31, 2019By: American Dental Association, American Student Dental Association. The American Cancer Society estimates there will be 53,000 new cases of oral and oropharyngeal cancer in 2019...
Read more
What to do for healthy teeth and gums?
March 25, 2019By: Jennifer Berry, Medical News Today Good oral hygiene is necessary to keep teeth and gums healthy. But, take note that oral health is more than avoiding cavities and gum disease...
Read more
Tooth whitening – don’t gamble with your teeth
March 20, 2019By: Damien Walmsley, The Conversation Are you one of those people who are dissatisfied with the color of our teeth? Have you tried to use some DIY methods and over-the-counter whitening products to whiten your teeth? If so, here are some recommendations from The Conversation to know if it is safe to continue. The Woodview...
Read more
Teeth Grinding: Causes and Preventative Care Steps You Can Take
March 15, 2019Whether you’re stressed or just anxious, teeth grinding, also known as bruxism, comes in many shapes & forms. And while the occasional grinding doesn’t hurt...
Read more
Receding Gums: Are Your Teeth in Peril?
March 10, 2019No cavities, no problem, right? Wrong! Even the straightest and whitest of teeth can fall prey to a serious case of receding gums, a common condition that can sneak up and do some damage before many individuals realize it’s even a problem. While a surefire way to detect and treat it is with regular visits...
Read more
The Mouthwash Mistake You Could Be Making
March 05, 2019It can freshen up your breath faster than brushing, but does mouthwash really make a big difference when it comes to your oral health? You may be surprised to find that looks–or in this case, smells–can be deceiving! Oral rinses are not created equal, and if you’re not careful, some can actually be more harmful...
Read more
Cranberries and blueberries – why certain fruit extracts could provide the key to fighting tooth decay
February 28, 2019By: Dental Health Org. New research shows that dark berries such as cranberries and blueberries contain nutrients...
Read more
Choosing the Right Professional Teeth Whitening Treatment
February 22, 2019When you want to whiten your smile, there are typically two options: drugstore kits or professional treatments. While some opt for the former...
Read more
8 Everyday Habits That Harm Your Smile
February 17, 2019Your teeth are supposed to last a lifetime. But some common habits could be reducing the durability of your teeth without you even realizing it. By recognizing the habits that can compromise the structure and health of your smile, you can take steps to protect it. 1. Avoiding Regular Dental Care Many individuals skip regular...
Read more
The Wise Patient’s Cheat Sheet on Wisdom Teeth Removal
February 12, 2019There’s no way around it: the time has come for your wisdom teeth to be extracted. According to the horror stories out there, you are in for nothing but non-stop agony, but you don’t have to share the same fate! Being proactive and fully prepared for what happens during and after surgery can minimize the...
Read more
Mind Your Meds: 6 Ways Medicine Can Sabotage Your Smile
February 07, 2019Be honest: do you take the time to read through the lengthy medical pamphlets attached to your medications? If you thought the warning label on the back...
Read more
High-Tech Toothbrushes: Is It Worth Going Electric?
February 02, 2019The verdict is in: electric toothbrushes are here to stay, and they mean business for your teeth! By now, you’ve probably seen them on the shelves, on TV or in magazines. Dentists endorse them, and most are ADA-approved — but if you still swear by your manual toothbrush, these benefits just might convince you otherwise...
Read more
Bye-Bye, Buck Teeth! How to Overcome an Overbite
January 28, 2019“Overbite”, “overjet” or simply “buck teeth”– protruding teeth can go by many names, but “pretty” isn’t one of them. And they aren’t comfortable either; upper teeth that extend well past the lower teeth can often make it difficult to close the mouth, chew or speak easily. It’s a common condition, but not one that people...
Read more
Not a Fan of Flossing? Try These Alternatives.
January 23, 2019First there was the toothpick, then there was floss, and now there are a bevy of new dental tools making their way to the shelves of your local stores. Why the need to keep innovating? Simply put: plaque removal is just not fun…but these alternatives sure help! For those fed up with flossing...
Read more
Xylitol: The Sweetener You and Your Dentist Will Love
January 18, 2019Consider this a major score for your sweet tooth: dentists are taking back that hard and fast rule that gum and candy rot your teeth! A sweetener called Xylitol makes it possible to enjoy such treats guilt-free, while actually fighting cavities along the way. For those who have long kept the candy aisle off limits...
Read more
Why does my tooth still hurt after a filling?
January 13, 2019By: Jennifer Berry, Medical News Today ? Is tooth sensitivity after a filling normal? Learn the reasons why it occurs, treatments to help relieve tooth sensitivity, and when to see us viaMedical News Today! The Woodview Oral Surgery Team A filling is a dental procedure that involves a dentist cleaning away any decay from the tooth...
Read more
Toothbrushes 101: How to Choose and Care for Your Toothbrush
January 08, 2019When it comes to taking care of your teeth and keeping your smile looking great, your toothbrush plays an essential role. But, how much thought do you actually...
Read more
What to do for healthy teeth and gums
January 03, 2019By: Jennifer Berry, Medical News Today Good oral hygiene is necessary to keep teeth and gums healthy. But, take note that oral health is more than avoiding cavities and gum disease. Research has shown that there is an association between the health of a person’s mouth and their overall health. Follow these tips from Medical News...
Read more
Christmas Foods to Avoid for Fresh Breath
December 24, 2018By: Capitol Hill Times ? The holidays bring lots of good food, drink, and socializing, but sometimes the conversations may be short due to what you’re eating. Dr. Harold Katz, developer of the TheraBreath line of oral products and widely recognized as “America’s Bad Breath Doctor” says there are certain holiday foods to avoid – if you don’t...
Read more
Removing plaque and tartar from teeth
July 08, 2018By: Jamie Eske, Medical News Today The buildup of plaque tartar on the teeth can cause bad breath, tooth decay, and gum disease. However, several simple home remedies can help treat and prevent plaque and tartar. Learn them via Medical News Today! The Woodview Oral Surgery Team Plaque is a soft, sticky film that builds...
Read more
What can cause gum pain?
July 03, 2018By: Rachel Nall RN MSN, Medical News Today The gums are soft, fleshy tissue that supports and protects the teeth. Gum pain can be a sign of irritation, infection, or injury to the gums and teeth. Medical News Today discussed some of the possible causes of gum pain, treatment, home remedies, prevention, and when to...
Read more
Breastfeeding: 6 Things Nursing Moms Should Know About Dental Health
June 29, 2018By: Mouth Healthy, American Dental Association (ADA) ? Breastfeeding can help your baby’s body fight infections...
Read more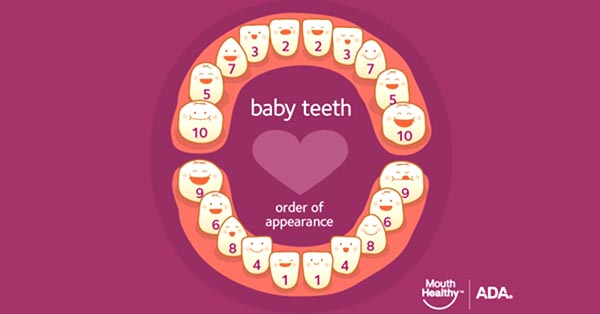
Baby Teeth
June 24, 2018By: MouthHealthy, American Dental Association (ADA) ? If you think your baby’s toothless smile is cute, just wait until their first few teeth make an appearance! After that first tooth comes in, don’t forget to follow these key takeaways from the American Dental Association to care for your baby’s oral health! The Woodview Oral Surgery Team...
Read more
Which comes first, brushing or flossing? New study shows that we should clean between our teeth before brushing
June 20, 2018By: George Bushell, Oral Health Foundation Brushing may come before flossing in the dictionary, but it shouldn’t when it comes to our teeth...
Read more
Kids, You May Be Using Too Much Toothpaste, CDC Suggests
June 15, 2018By: Bruce Y. Lee, Forbes. How do you know if your kids are using too much toothpaste? And how much is the recommended amount that we should give them? Use this guideline from Forbes! The Woodview Oral Surgery Team How do you know if you are using too much toothpaste? If your body is covered in...
Read more
How long does it take to recover from a wisdom tooth extraction?
June 10, 2018By: Claire Sissons, Medical News Today Are you planning to visit us for a wisdom tooth extraction soon? ? Before you come in, get yourself prepared with these tips from Medical News Today! The Woodview Oral Surgery Team Wisdom teeth removal is one of the most common dental surgeries. It can take up to 2 weeks to recover...
Read more
Is Water Flossing the Perfect Tool for Better Oral Health?
June 06, 2018By: Jacqueline Fallon, The Dental Geek According to the Center for Disease Control and Prevention’s ( CDC ) Oral Health report, over 90% of Americans have had at least one cavity,and one in four has untreated tooth decay. Meanwhile, around half of all adults above the age of 30 have gum disease. Dentists recommend brushing and flossing...
Read more
Why do our kids have tooth decay?
June 02, 2018By: Alvin Danenberg, DDS, DrBicuspid.com DYK that the primary reasons our kids have tooth decay and gum disease are because of nutritional deficiencies? Some of the top causes related to this issue are acidic and sugary drinks, compromised gut bacteria, and a sedentary lifestyle. ??⚕️ Worried about your kids? DrBicuspid has some advice! The Woodview Oral Surgery Team Our...
Read more
Dentists say this common ingredient could be messing with your mouth
May 28, 2018By: Zoe Weiner, MSN The best part of brushing and swishing mouthwash (aside from the whole “no gum disease or cavities” thing)...
Read more
DIY braces? Orthodontists say to think twice before straightening your teeth solo
May 23, 2018By: Joanna Clay, University of Southern California; Medical Xpress. Are you considering straightening your teeth through DIY braces? If so, you might want to check out this article via Medical Xpress – Medical and Health News before jumping into the decision! The Woodview Oral Surgery Team A couple of years ago, the story of a college student 3-D printing his...
Read more
How can boosting Your Vitamin And Mineral Intake Protect Your Smile?
May 19, 2018By: Lucy Wyndham, Dental News Everyone knows that eating a good mix of vitamins and minerals is vital for optimum health, but did you know that these nutrients are just as essential for your dental health? The Woodview Oral Surgery Team According to the Centers for Disease Control and Prevention, 47.2% of American adults have some form of...
Read more
What your dental hygienist wants you to know about the importance of oral health
May 15, 2018By Heather Jackson, Loma Linda University Health Whether the topic is flossing and brushing or baby teeth and cavities, your dental hygienist has important advice. Remember these key takeaways from Loma Linda University Health to help you properly care for the gateway to the rest of your body. The Woodview Oral Surgery Team Whether the topic is flossing and brushing...
Read more
7 Soft Recipe Ideas Dental Patients Often Overlook
May 10, 2018By:Anna Medaris Miller, US News Distract yourself from pain – and expedite healing – by getting creative in the kitchen. Here are some soft food ideas from USNews! The Woodview Oral Surgery Team RX: Soft foods As if getting your wisdom teeth out, your tonsils removed or your mouth otherwise manipulated, injured or operated on isn’t...
Read more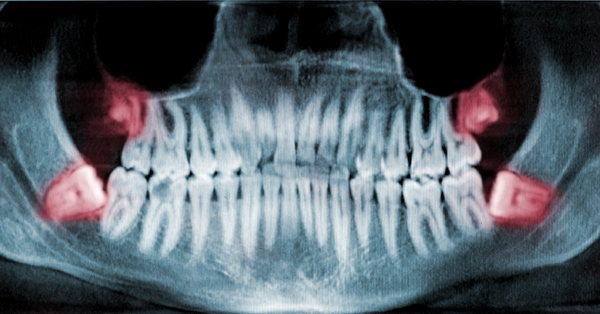
When Should I Have my Wisdom Teeth Removed?
May 05, 2018By: Consumer Guide to Dentistry Wisdom teeth removal is a common oral surgery, but as is the case with tonsils, their removal is not always necessary. This begs the obvious question: When should wisdom teeth be removed? Learn more! The Woodview Oral Surgery Team Wisdom teeth — also referred to as third molars — are typically the...
Read more
How Seniors Can Prevent Tooth Loss?
April 30, 2018By Lucy Wyndham, Dental News You may have noticed that tooth loss is very common during aging, but are there ways you can do to prevent it? Tips shared by Dental News! The Woodview Oral Surgery Team Sadly, about 27% of seniors over the age of 65 have no remaining teeth, as per […]
Read more
Beyond tooth decay: why good dental hygiene is important
April 26, 2018By: David McNamee, Medical News Today Most of us are aware that poor dental hygiene can lead to tooth decay, gum disease, and bad breath, but not brushing your teeth could also have consequences for more serious illnesses. Check out the other diseases you can acquire with poor oral hygiene via Medical News Today...
Read more
What to do to keep gums healthy
April 22, 2018By: Jenna Fletcher, Medical News Today Practicing good oral hygiene is the most important action that a person can take to prevent and treat gum disease. Most people tend to overlook their gums when it comes to oral health and focus on getting a bright, white smile instead. However, healthy teeth require healthy gums...
Read more
What causes a bump on the roof of the mouth?
April 19, 2018By: Elaine K. Luo, MD, Medical News Today A bump on the roof of the mouth can be worrisome, especially if it does not go away quickly. Most causes of a bump on this part of the body are easily treatable, but it may also indicate a more serious underlying condition....
Read more
Why is the roof of my mouth swollen?
April 14, 2018By: Jenna Fletcher, Medical News Today Many conditions may cause a swollen roof of the mouth, including sores, dehydration, and mucus buildups. In this article via Medical News Today, learn about six causes of a swollen roof of the mouth, and possible treatment or home remedies. The Woodview Oral Surgery Team The roof...
Read more
What Anglo Saxon teeth can tell us about modern health
April 10, 2018By: University of Bradford, Science Daily Evidence from the teeth of Anglo Saxon children could help identify modern children most at risk from conditions such as obesity, diabetes, and heart disease. Learn more about these critical findings via ScienceDaily. The Woodview Oral Surgery Team Researchers from the University of Bradford found that analysis of milk...
Read more
Does teething cause a baby to vomit?
April 06, 2018By: Karen Gill, MD, Medical News Today Vomiting and fever may sometimes accompany teething. Teething is a normal part of a child’s development that may cause some discomfort. However, it is unlikely that teething is a direct cause of vomiting. The Medical News Today shares other possible causes of vomiting and discusses how to relieve the...
Read more
Advanced dental technology: Don’t get left behind
April 02, 2018By: Dental Economics. The advancement of dental technology can lead to high-quality care to dental patients. Along with this upgrade, we ensure to provide efficient practice for your comfort and benefit. The Woodview Oral Surgery Team If you’ve been keeping up with developments in oral health care over the past decade...
Read more
Nature vs. Nurture: Dental Problems Parents Pass Down To Children
March 29, 2018Parents, in particular, want to know: does DNA predetermine dental health? The Woodview Oral Surgery Team It’s the classic nature vs...
Read more
After the Removal of Multiple Teeth
March 25, 2018By: Orlando Oral Facial Surgery ? From the primary operation to its effect, the removal of multiple teeth is quite different from the extraction of just one tooth. Check out these guidelines on what to do after the teeth extraction to prevent any complications from occurring...
Read more
Mystery Solved: The Story on Canker Sores
March 20, 2018Anyone who’s ever had mouth sores can attest to the fact that they are just as embarrassing as they are painful, but simply suffering through them does...
Read more
How Safe Are Dental X-Rays?
March 15, 2018By: 123Dentist. As long as dental x-rays are used properly together with necessary safety precautions, its effect is extremely safe. Discuss the use of this device with your dentist so he can evaluate the factors if you need one...
Read more
How Stress Might Be Ruining Your Teeth
March 11, 2018By: Kelsey Lindsey, Washingtonian. You may know that stress can cause upset stomachs and headaches, but did you know it can cause tooth decay?...
Read more
Traumatic Dental Injuries
March 08, 2018By: Oral and Facial Surgery Institute. A traumatic dental injury is a serious condition which requires an immediate dental consultation. A mild pain does not mean you’re safe. There is a chance that the affected area may only be made visible through a thorough exam...
Read more
Five Tools Everyone In the Oral Surgery Industry Should Be Using
March 08, 2018By: Dentaltown. The dental industry is innovating, too! As a product of innovation, we’ve got 5 recommendable tools...
Read more
Oral Surgery Basics
February 28, 2018By: Consumer Guide to Dentistry. An oral surgeon is skilled to treat different mouth conditions. They provide services suitable for your needs! The Woodview Oral Surgery DC Team...
Read more
Advances in Dental Care: What’s New at the Dentist
February 25, 2018By: WebMD. With technological advancement, tooth restoration was made easy. Thanks to these modern tools used in dental practices today, there are a lot of good options to keep our teeth beautiful...
Read more
Ibuprofen And Acetaminophen Together May Give Profound Pain Relief With Fewer Side Effects After Dental Surgery
February 21, 2018By: Colgate. A study conducted by dental experts shows that combining Ibuprofen and Acetaminophen...
Read more
Pain Relief for Wisdom Teeth Removal
February 16, 2018By: Adeola Abisogun, Livestrong. Pain may occur after a wisdom tooth removal. To avoid this and prevent the occurrences of complications, follow your dentist’s guidelines for a best dental experience! The Woodview Oral Surgery Team...
Read more
Common Types of Oral Surgeries and What You Can Expect
February 12, 2018By: Dental Pointe. From wisdom tooth removal to a reconstructive operation, each oral surgery type has different functions. Determine which of them is suitable for your needs. The Woodview Oral Surgery Team...
Read more
Complications During and After Surgical Removal of Third Molars
February 07, 2018By: by Hans Ulrich Brauer, DDS, Dr. Med Dent, MA; Robert A. Green, DDS, MD, Msc, FRCD(C); Bruce R. Pynn, Ms, Oral Health Group. There are recent studies which identify risk factors during and after removal of third molars.
Read more
What To Eat After Tooth Extraction
February 03, 2018By: Amy Freeman, Colgate. It is very important to plan the right kinds of food after your tooth extraction. They can ease your recovery and aid in faster healing...
Read more
Top 3 Reasons for Kids Dental Surgery
January 30, 2018By: Main Street. Even children are not free from dental surgery if their oral hygiene is neglected. Guide them to a healthy oral routine and this will be avoided...
Read more
Gray and Black Market Dental Products: Are You at Risk?
January 26, 2018By: Consumer Guide to Dentistry ? Have you heard about the gray and black market before? To avoid the risks and harmful effects of using these products...
Read more
A Guide to Common Dental Problems
January 26, 2018By: Sally Solo, Real Simple ? Keep this guide to common dental problems handy so you’ll achieve the perfect smile everybody would want to see...
Read more
Cavities: How and Why Do Dentists Fix Cavities for Children?
January 18, 2018By: 123Dentist ? Kids are not safe from cavities. This condition should receive immediate treatment before it causes pain to your child. The Woodview Oral Surgery Team Though children are using a set of teeth they will eventually lose...
Read more
Is Dental Sedation Safe For Kids?
January 15, 2018By: Jenny Green, Colgate. Parents also play an important role during the dental sedation procedure. Prepare your child and follow the guidelines to gain positive results. The Woodview Oral Surgery Team Safety is parents’ top consideration when it comes to their child receiving dental sedation...
Read more
Dental Implant Process Take Time
January 11, 2018By: Prestige Oral Surgery. If a dental implant is your best tooth replacement option, the length of this procedure depends on your oral health.
Read more
Wisdom Teeth Removal: What Adults Should Expect
January 07, 2018By: WebMD. Knowing the things you should expect from your tooth extraction procedure is one effective way to get prepared...
Read more
Soda After Wisdom Teeth Removal
January 02, 2018By: Brynne Chandler, Livestrong. Diarrhea may occur after the wisdom tooth extraction, however, this is preventable...
Read more
Needle Phobia and Fainting
December 26, 2017By: Dental Fear Central ? Do you feel anxious at the sight of needles? There is something you can do and your dentists can help you, too!...
Read more
Toddlers having teeth out because parents won’t take them to dentist
December 20, 2017By: Laura Donnelly, The Telegraph UK. Most often, parents think their toddlers are too young to visit the dentist. The truth is, children should practice good oral habits as early as their first tooth appears...
Read more
8 Foods to Eat After You Have Your Wisdom Teeth Removed
December 15, 2017By: Riverrun Dental ? Eating the right kinds of food is highly recommended to aid in recovery. Aside from faster healing, they are healthy...
Read more
Sedation Dentistry: Anesthesia Administered by a Medical Doctor
December 10, 2017By: iCare Oral Surgery. Sedation dentistry is a relaxing dental procedure you should not be afraid of. Don’t hesitate to discuss your fear with your dentist so he can give you options for a better dental experience...
Read more
Teeth Whitening & Health: Are Coffee and Tea Bad for Teeth?
December 05, 2017By: Park Avenue Dental ☕ Can’t start your day without coffee or tea? This article helps you figure out its impact on your teeth...
Read more
Teeth Whitening: How it Works and What it Costs
December 01, 2017By: Your Dentistry Guide ? Tooth discoloration is a common problem that also affects our smile. Find the best teeth whitening option for you and bring back your confidence...
Read more
Effects Of Smoking On Teeth And How To Kick The Habit
November 27, 2017By: Donna M. Rounsaville, Colgate. It’s No Smoking Day, a holiday we definitely endorse! Smoking takes a toll of smoker, and their teeth.
Read more
Dental paresthesia: Nerve damage as a complication of wisdom tooth extraction or dental injection.
November 22, 2017By: Animated-Teeth.com ? Have you heard about Dental Paresthesia? Discover its signs, symptoms, causes, and treatment before you’re at risk...
Read more
What Are the Most Common Dental Problems?
November 18, 2017By: Tammy Davenport, Verywell Health. Understanding common dental problems allow you to take preventive measures to keep a healthy smile. Remember, your mouth can tell you many things about your body...
Read more
What Are the Common Side Effects of Dental Implant Surgery?
November 14, 2017By: Coastal Jaw ?Dental implants are proved and tested to be safe. There may be some minimal side effects within a week after the surgery...
Read more
Recovering from oral surgery
November 10, 2017By: Delta Dental ? Let’s work together to help you get back to your normal routines after an oral surgery. These tested general guidelines will help ease your recovery...
Read more
New intraoral scanner challenges the dental market in 2017 – Heron™ IOS
November 07, 2017By: Dental Products Report. Good news for everyone! 3DISC has announced a new 3D scanner designed for dentists to make digital impressions. This is another product created to improve the modern dental practice and provide an efficient service to dental patients...
Read more
Ancient Pompeiians Had Good Dental Health But Were Not Necessarily Vegetarians
November 05, 2017By: Kristina Killgrove, Forbes ? Despite the lack of the modern technology, the Pompeiians were still able to keep their teeth healthy and strong. Want to discover their secret?...
Read more
Dental Implant and Dental Bridge
November 02, 2017By Prestige Oral Surgery. Want to know the best tooth replacement method suitable for your condition? Understand the difference between dental implants & dental bridges before you decide...
Read more
Tooth extraction healing. – How long does it take? / What can you expect? / Precautions and restrictions.
October 31, 2017By Animated-Teeth.com ⏳ Many factors contribute to the time frame of your tooth extraction recovery. Read more about the healing process! The Woodview Oral Surgery Team Once your tooth’s extraction process has been completed...
Read more
What Is Oral Surgery and How Is It Used?
October 28, 2017By Verywell ?From tooth extraction to the treatment of diseases, oral surgery is a common procedure used to correct different mouth conditions...
Read more
What Is Oral Surgery And Why Would I Need It?
October 28, 2017By The Happy Tooth. You might need an oral surgery in certain cases. Distinguish its difference from the maxillofacial surgery and when might you need them...
Read more
Oral treatments and dental health > Caring for Teeth
October 26, 2017By dentalhealth.org Proper care of our teeth is essential to prevent different gum diseases. Follow these tips to keep your mouth healthy! The Woodview Oral Surgery Team Why are my teeth so important...
Read more
The 30 Best Foods for Healthy Teeth and Gums
October 23, 2017By nano-b. No matter how strict your oral hygiene routine, if you don’t watch your diet you are still putting your oral health at risk...
Read more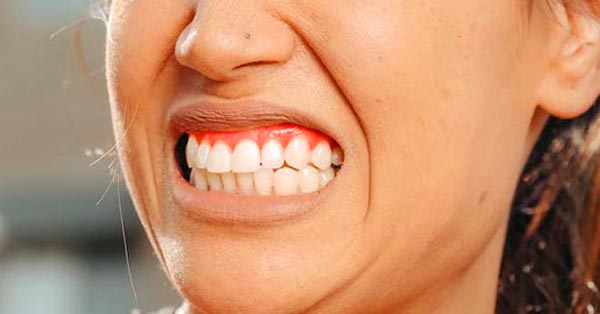
Gum Disease
October 20, 2017By Colgate Discover the causes, symptoms, diagnosis, and ways to prevent the gum disease from damaging your oral health. The Woodview Oral Surgery Team Definition Gum disease is an inflammation of the gum line that can progress to affect the bone that surrounds and supports your teeth. The three stages of gum disease — from […]
Read more
Recovery After Oral Surgery
October 18, 2017By Shawn Watson, Very Well ?Always follow the post-operative instructions of your dentist for your optimum recovery! The Woodview Oral Surgery Team Recovery should be your number one concern after oral surgery. Always follow the post-operative instructions provided by your surgeon or dentist to prevent any risk of infection or trauma to the surgical site. Follow […]
Read more
Wisdom Teeth Anesthesia Options
October 15, 2017By: Donna Pleis, Colgate Can you opt for a PAINLESS wisdom tooth removal? Find out how. The Woodview Oral Surgery Team If your dentist recommends removing your wisdom teeth because they’re decayed or aren’t erupting correctly in your mouth, don’t panic. As daunting as it sounds to have teeth extracted, this common process may […]
Read more
Dentists Use Computers to Make Dental Implants
October 12, 2017By WNDU ?️Technology has even invaded the dental industry. One of its advantages is the creation of dental implants. The Woodview Oral Surgery Team When traditional dentistry and reconstruction failed, some people went high-tech. It’s the stuff of science fiction, now showing up in dental offices. Dentists and prosthodontists are using computers to make teeth, […]
Read more
The 25 Worst Foods and Drinks for Your Teeth and Gums
October 10, 2017By nano-b ?️Some of the foods and drinks we consume can also affect the health of our teeth. Time to learn about their negative effects. The Woodview Oral Surgery Team The Importance of Your Diet for Your Teeth’s Health Since you are here, you probably know how important your oral health is for your overall […]
Read more
Everything You Need to Know about Sensitive Teeth
October 07, 2017By nano-b ?Feeling a sharp pain in your tooth every time you eat your favorite food? Don’t let a sensitive tooth ruin the moment. The Woodview Oral Surgery Team Just being alive can cause sensitive teeth We all know that moment when we are about to sip from our favorite tea and instead of enjoying […]
Read more
The Surprising Connection Between Your Oral Health and Your Overall Well-being
October 05, 2017By: The Nano-B Team ?Your oral health is the reflection of your overall well-being. Find out why! The Woodview Oral Surgery One legend tells the story of young Krishna, a Hindu God, eating fallen apples although he was told not to. He got some mud in his mouth while he was doing it. His mother […]
Read more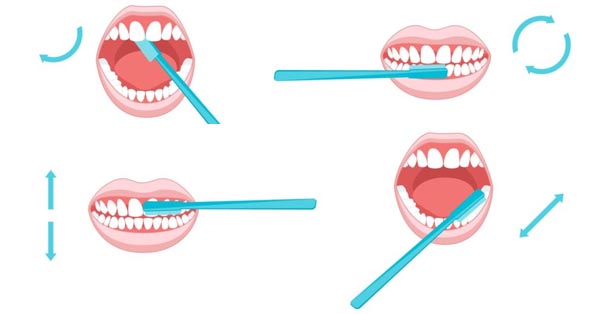
How to Properly Brush your Teeth
October 03, 2017By: The Nano-b Team ?Simply brushing your teeth is not enough. Include these PROPER techniques in your habit. The Woodview Oral surgery Team It seems incredible how universal the habit of teeth brushing is all over the world. It might very well be the most widely practiced health habit people do on a daily basis. This fact […]
Read more
Your teens may think that they don’t need you anymore, but they’ll always need their teeth!
September 30, 2017By: Campaign for Dental Health, American Academy of Pediatrics Your teens may think that they don’t need you anymore, but they’ll always need their teeth! They will thank you for setting the foundation for good oral health by modeling the best practices and having them see a dentist regularly. Read more here! If you need […]
Read more
New Implant Advancement Hopes to Lower Risk of Infection
September 28, 2017By: KU Leuven, Oral Health Group ? New research has developed a dental implant that can gradually release drugs from a built-in reservoir which helps prevent and fight infections: Visit our website to learn more about dental implants: http://buff.ly/2eYfjKE ...
Read more
The Evolution of the Toothbrush
September 25, 2017By: Irma Wallace, Infographic Journal [INFOGRAPHIC] ? Can you imagine brushing your teeth with horsehair?! Take a look at just how far the toothbrush has come. The Woodview Oral Surgery Team Attention to dental hygiene dates all the way back to 3500 BCE with the Chew Stick in Egypt and Babylonia...
Read more
Can You Get Through This Post Without Wanting To Brush Your Teeth?
September 23, 2017By: Kelly Oakes, BuzzFeed ? CHALLENGE: Try getting through this disturbing article without wanting to brush your teeth! The Woodview Oral Surgery Team Here’s what your teeth look like up close and personal with a scanning electron microscope...
Read more
New material used in molar extraction sites optimizes bone regeneration and dental implant stability
September 20, 2017By: Journal of Oral Implantology ? [Good to know]: New material used in molar extraction sites optimizes bone regeneration and dental implant stability. Curious to learn more?...
Read more
The complete guide to great oral health
September 18, 2017By: Southcommon Dental ? Besides brushing, here are other important steps to maintain great oral health. Check out the complete guide here. The Woodview Oral Surgery Team Take a moment to think about your own oral health...
Read more
An Easy Recipe for A Happy and Healthy Childhood
September 15, 2017By: ilikemyteeth.org ? It’s as easy as 1, 2, 3! Help your children stay away from pain from dental caries or abscessed teeth, give your children a happy and healthy childhood...
Read more
5 FOODS FOR HEALTHIER GUMS
September 12, 2017By: Listerine ? Beyond just limiting the sugary sweets and harsh acidic foods in your diet, incorporate foods that are good for your gums, too! The Woodview Oral Surgery Team Routine brushing, flossing, and rinsing keep your mouth in good health...
Read more
A Year of Oral Health Guidance in Review
September 10, 2017By David Cavano, Dental Health ? Summer is here! Here’s some oral health guidance from the past year to help you understand what new information is available and which tried-and-true practices still stand...
Read more
Consider the Evidence: Fluoride For Healthy Futures
September 07, 2017By: Mirissa D. Price, Huffington Contributor [OPINION]: Fluoride represents a major step toward not just treatment, but also prevention in oral health. Fluoride for healthy futures!...
Read more
End of fillings in sight as scientists find Alzheimer’s drug makes teeth grow back
September 05, 2017By Sarah Knapton, Telegraph ❗️ Fillings could be sent to the history books after scientists discovered that a drug, already in trials for Alzheimer’s patients, can encourage tooth regrowth and repair cavities!...
Read more
LATEST TECHNOLOGY MAKES DENTAL IMPLANTS EASIER FOR PATIENTS – AND SURGEONS
September 02, 2017By Dental Asia ? Good news!! The latest technology will make dental implants easier for patients and surgeons, which means no incisions, minimal discomfort and little disruption!...
Read more
Busboys and Poets in Anacostia May Not Open Until 2018
August 30, 2017by Nena Perry-Brown Six months ago, construction began at the future site of the first Busboys and Poets restaurant east of the Anacostia River...
Read more
Top 10 New Technologies in Dentistry
August 27, 2017By 123Dentist Check out the top 10 new technologies in dentistry treatment: VLscope, digital X-Rays, invisalign, laser dentistry and more!http://buff.ly/2vbMsc4 If there’s a need...
Read more
Poor oral health contributes to 6 common diseases
August 25, 2017By Lori Alton, NaturalHealth365 ? Did you know chronic inflammation of the gums can affect your entire body? Here are the top 6 diseases you can contract from poor oral health...
Read more
What would a month without sugar mean to your child’s teeth?
August 23, 2017By Campaign Dental Health What would a month without sugar mean to your child’s teeth? Check out the results of the project “A Month Without Sugar” and consider making a plan for yourself and your family...
Read more
The Power of Sour on Your Teeth
August 20, 2017By Media Planet You know that weird coating you get on your teeth and tongue when you eat certain candies? Sour foods can be just as damaging to your teeth as sweets due to their high acidity!...
Read more
Foods That Fight Mouth Bacteria
August 20, 2017By SFGATE FUN FACT: Apples help kill bacteria in the mouth that causes bad breath! Learn more about other foods that fight bacteria below...
Read more
5 natural remedies for gum disease that are better than toothpaste or mouthwash
August 13, 2017By The Hearty Soul Tell your friends that there are 5 natural remedies for gum disease that are better than toothpaste or mouthwash, and yes, one of them is chocolate!...
Read more
Why Sharks Don’t Get Cavities
August 10, 2017By Megan Garber, The Atlantic Should sharks be our role models for oral hygiene? Learn about the two species with “toothpaste-teeth”! The Woodview Oral Surgery Sharks live lives that are, to human sensibilities, mostly unenviable...
Read more
The Secret To Better Teeth Found In Beer Breweries
August 07, 2017By Jason Tetro, Popular Science Are beer hops the secret to superior oral health? The Woodview Oral Surgery Team On St. Patrick’s Day, millions of people worldwide will raise their beer glasses and...
Read more
When It Comes to Oral Health, We Can Learn Something from the Beavers
August 04, 2017By Youth Health. When it comes to understanding tooth decay, a group of researchers is saying, “Leave it to beavers.” Researchers from Northwestern University have discovered something remarkable about the oral health of beavers...
Read more
How Chewing Gum Can Help Your Oral Health
August 02, 2017By Jason Tetro, Huffpost Is chewing gum good or bad for your teeth? Let’s settle the debate once and for all. The Woodview Oral Surgery Team The question has plagued dental professionals for years...
Read more
Hi-tech ‘triple toothbrush’ can clean your mouth in just ten seconds
July 30, 2017By MARK PRIGG FOR DAILYMAIL.COM For those who simply don’t have time to brush their teeth in the morning, help is at hand...
Read more
Chocolate: A Superfood for Your Teeth
July 27, 2017By Ask the Dentist Who says chocolate isn’t good for you? The antibacterial effects of chocolate can help protect against tooth decay. Sounds too good to be true? Read more on why you can justify your chocolate cravings below...
Read more
Happy International Women's Day!
March 10, 2017Our amazing staff, dressed in red, gave all of our patients at the DC office red roses yesterday! Happy International Women’s Day!...
Read more
"Can Drinking Lemon Water Damage My Teeth?"
March 10, 2017By David Wolf, DavidWolf.com ? Sadly, that refreshing water with citrus fruit in your office can do more harm than you think!...
Read more
These 4 Natural Remedies Will Repair Receding Gums
March 10, 2017By Brandon Richard, DavidWolf.com ? Need ideas on how to help receding gums? These four natural remedies may help: http://buff.ly/2djJRGg ...
Read more
Dental Implant 101
March 10, 2017You may be surprised to know that a lot happens in your mouth when you lose a single tooth! Learn more in our short explainer video here: http://bit.ly/2daWYtl ...
Read more
Can You Handle The Tooth? 10 Things You Didn't Know About Teeth
March 10, 2017By Amanda Green, Mental Floss The average adult has 28 to 32 teeth, depending on their “wise” set of third molars or lack thereof...
Read more
Short On Time? This Hi-Tech 'Triple Toothbrush' Cleans In TEN Seconds!
December 01, 2016Now you definitely have time to brush! Check out this clip on how to clean your mouth in just 10 seconds with this brand new toothbrush technology...
Read more
"What Happens After My Tooth Extraction?"
November 20, 2016→ Here’s everything you need to know from Dr. Nkungula to help prepare for dental care after your visit: Post – Operative Mouth Care Care of the mouth following a surgical procedure is essential in the healing process...
Read more
College Student Made His Own Braces For $60, And His Teeth Look Fantastic
November 10, 2016By Kimberly Yam, The Huffington Post. Believe it or not, a college student 3D-printed his own braces for $60! Read below to learn more about this possible game-changer for the dental field...
Read more
Review: Everyone at this office was polite and professional
October 27, 2016“Everyone at this office was polite and professional. I was very impressed with the service I received. Like many others, I am terrified of oral surgery, the staff her gave me a new outlook because of their knowledge in their profession...
Read more
E-Cigarette Explosions Causing Serious Mouth Injuries
October 21, 2016E-cigarettes are sold under some 450 brands...
Read more
Busboys & Poets: Coming Soon to Anacostia
October 21, 2016We’re thrilled to hear that another restaurant is opening up...
Read more
Learn More About Dr. Nkungula
October 14, 2016Read more about Dr. Nkungula here ➤ http://buff.ly/2cSOH8U
Read more
Foods You Can Eat With Braces
October 07, 2016Now that you have your braces, how do you take care of them? It’s important for you to know how to properly take care of your braces...
Read more
Dental Sealants Decrease Risk of Tooth Decay
September 30, 2016Although tooth decay is largely preventable, it remains the most common chronic disease...
Read more
Happy Labor Day!
September 05, 2016[VIDEO] Curious to learn more about the history of Labor Day? Check out this video by the History Channel! ➤ http://buff.ly/2c7xCtt
Read more
Review: It's about time premium dental care comes to SE
August 06, 2016“I have to say that it is about time that premium dental care...
Read more
Why You Need to Brush Your Teeth Before Bedtime
July 21, 2016Do we really have to brush our teeth twice a day?...
Read more

Should You Have Your Wisdom Teeth Removed?
June 02, 2016Does the thought of getting your wisdom teeth pulled make you squirm? Let’s find out if you really need to get those teeth removed! ➤ http://buff.ly/1RlK9Ti
Read more
What Are Dental Implants?
May 23, 2016Curious about dental implants? Check out our simple explainer video so you can learn about how you can smile with 100% confidence ➤ http://buff.ly/22mJ85n
Read more
Review: "Love you guys!"
April 08, 2016“Upon walking in, the office was very welcoming. The staff was very knowledgeable, and warm. I was immediately escorted to the room, where the surgery was to take place (NO WAIT!)...
Read more



4.9 Stars
based on 134 reviews
5 Stars
based on 11 reviews
5 Stars
based on 11 ratings